Objective:
To investigate the effect of motor cortex stimulation (MCS) on central poststroke pain (CPSP) and the outcome predictors associated with medium- to long-term results.
Materials and Methods:
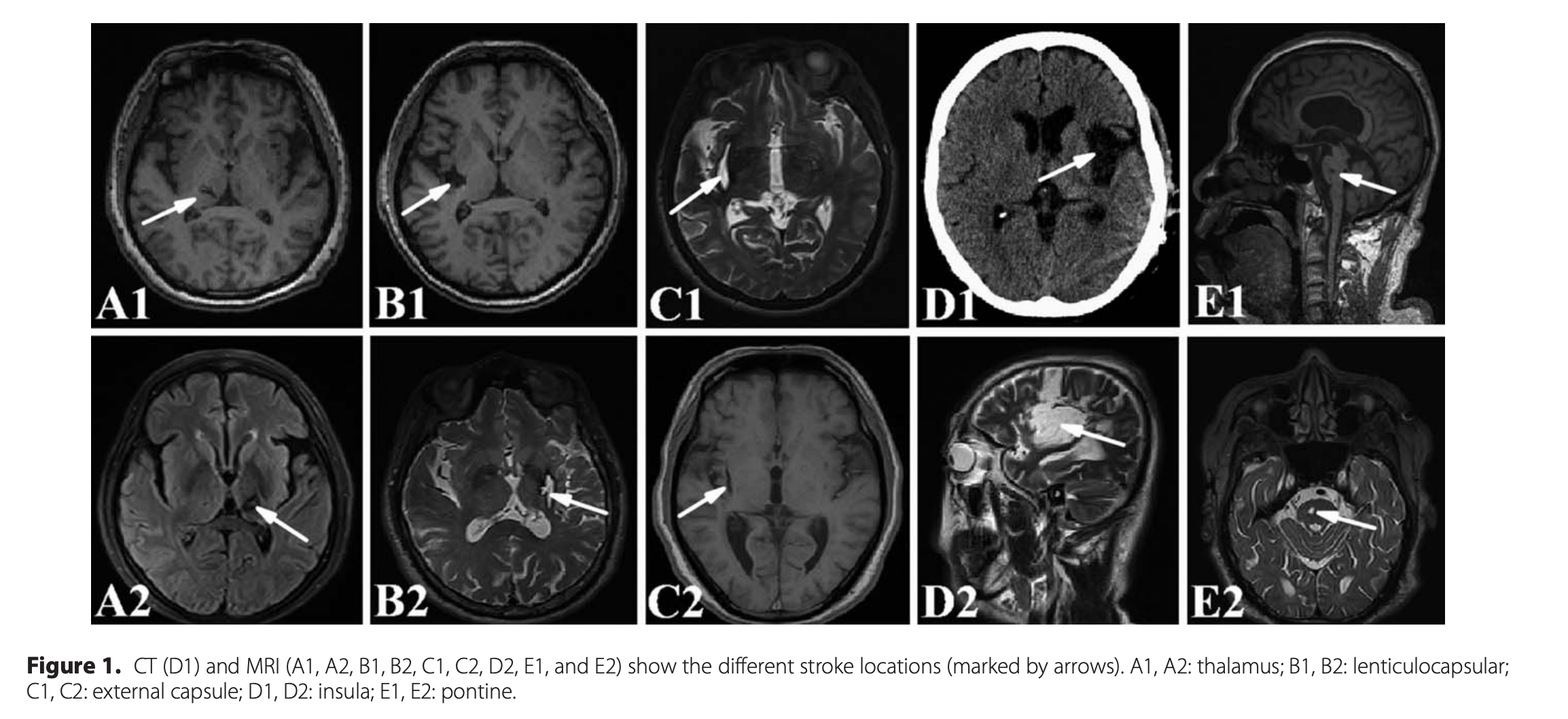
This is a retrospective review of 16 CPSP patients treated with MCS with a mean follow-up of 28.2 months. The pain intensity was assessed based on the visual analogue scale (VAS) before surgery and at various follow-up visits. An effective outcome was determined to be at least 40% pain relief. The type (hemorrhage or ischemia) and location (thalamus or non-thalamus) of the stroke, the location of the electrode (epidural or subdural), and preoperative repetitive transcranial magnetic stimulation (rTMS) results were analyzed to evaluate whether they are predictive of effective outcomes.
Results:
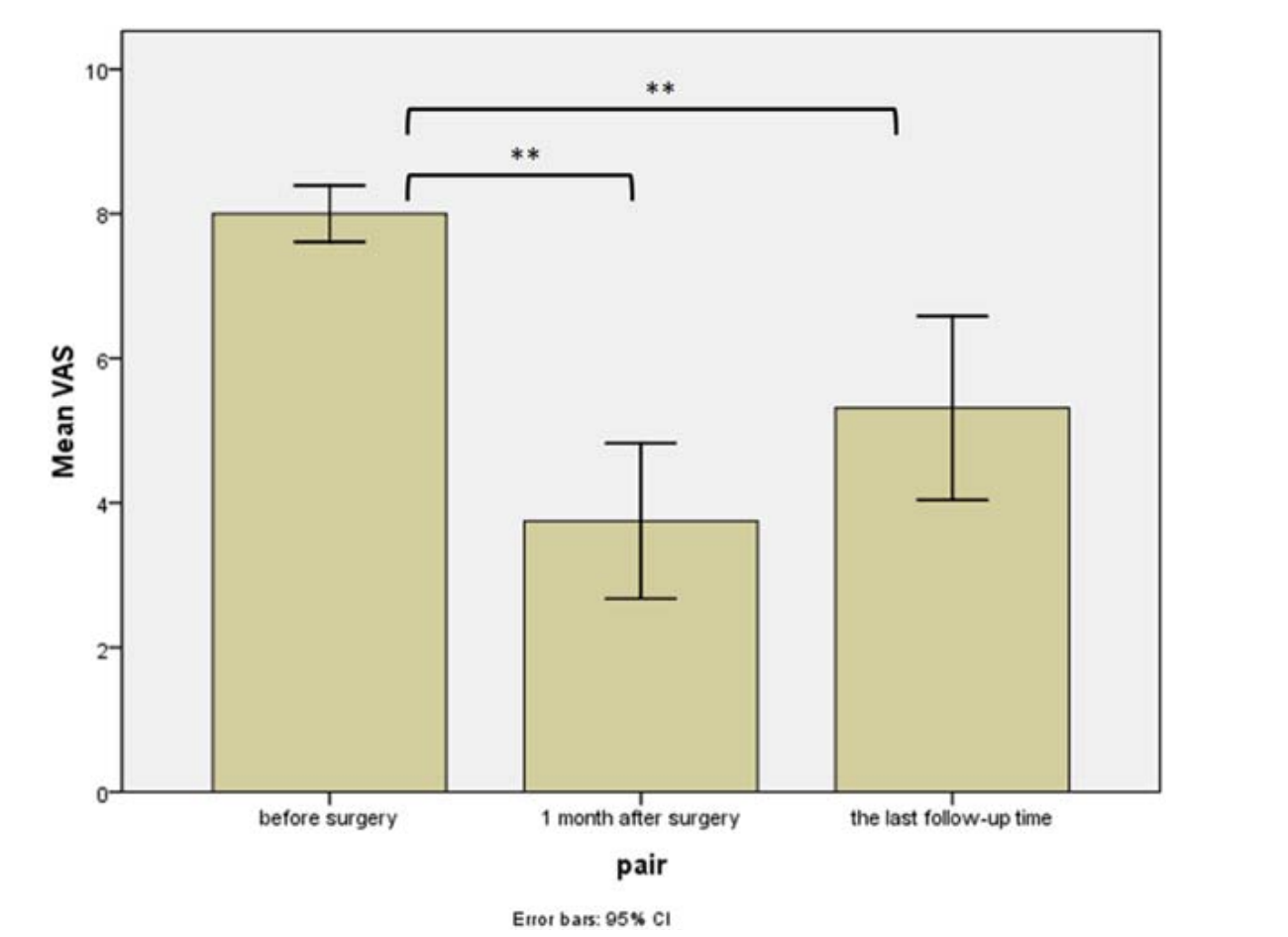
The mean VAS before surgery was 8.0 ± 0.7 compared with 3.8 ± 2.1 one month after surgery and 5.3 ± 2.4 at the last follow-up. There were no differences in the analgesic effects between the types of stroke (hemorrhage or ischemia), stroke location (thalamus or non-thalamus), or the location of the electrode (epidural or subdural). The association between preoperative rTMS and effective outcomes was significant with a positive predictive value of 0.8571 and a negative predictive value of 0.7778.
Conclusions:
Our results suggest that MCS significantly reduces the pain intensity of CPSP. The types of stroke (hemorrhage or ischemia), stroke location (thalamus or nonthalamus), and the location of the electrode (epidural or subdural) were not significant predictors of the analgesic effects of MCS. Preoperative rTMS might be helpful for screening candidates for MCS.